While aging services providers slowly move forward in implementing electronic health records, a lack of workflow redesign and adoption practices continue to hamper providers’ efforts to realize the full potential of these computerized systems. Chief among the challenges are 1) inconsistent and poorly designed training programs, 2) disconnects between old workflow patterns and new opportunities, 3) a lack of data governance structures, and 4) failure to embrace optimization opportunities.
1) Inconsistant and Poorly Designed Training Programs
Providers and vendors continue to waste significant resources during training and implementation phases by blasting webinar-based training to classrooms full of staff. Not only is this training style time-consuming and expensive, it is ineffective at building proficiency in users. Why is this important? Research has shown that adults learn much better when concepts are tied to the work they are expected to do. In the case of EHRs, the goal should be to have proficient users– in other words, staff are able to use the application effectively to do their job– as opposed to knowing a complex set of modules and screens.
By listening to and/ or watching a remote user walk through screens and screens of capabilities, staff are likely to retain very little once the training is completed. Instead, training should be developed and deployed around workflow and roles, using a well-designed simulation environment that closely matches the new system. The savings from this approach alone can make retaining an external, experienced EHR consulting firm cost-effective.
Once systems are implemented, providers should develop strong training programs that can be consistently provided to new staff. A reliance on web-based training modules leads to poor proficiency and increased variation in usage and data entry, as does training provided solely as part of a traditional floor orientation program. Instead, providers should take the time to develop (and keep updated) a training program that includes simulation, facility-specific guides, and leadership oversight to ensure continuity of information and practices.
2) Workflow Challenges
EHRs offer a tremendous opportunity to remove significant waste from operations. From hunting down charts to keeping documentation in one place, an EHR can bring order to chaotic paper charts. Because of this, new workflows oftentimes need to be developed to take advantage of these opportunities. Role for medical records, MDS nurses, billing staff and floor nurses all need to be examined to determine the most effective mechanisms for entering and maintain data in an EHR. The challenge is that even during an EHR build and design phase, paper-centric thinking reigns. This creates a bias towards old systems that leaves most implementations under-powered and underutilized.
Charting and review systems need to be assessed, as EHRs typically provide visibility into areas that previously required redundant systems to manage. Any parallel information systems being used after implementing an EHR should be carefully examined to ensure there isn’t a duplication of data or efforts occurring. Without direct assessment and action, it’s not uncommon for providers to waste 10-15% of their resources maintaining outdated or redundant systems and databases.
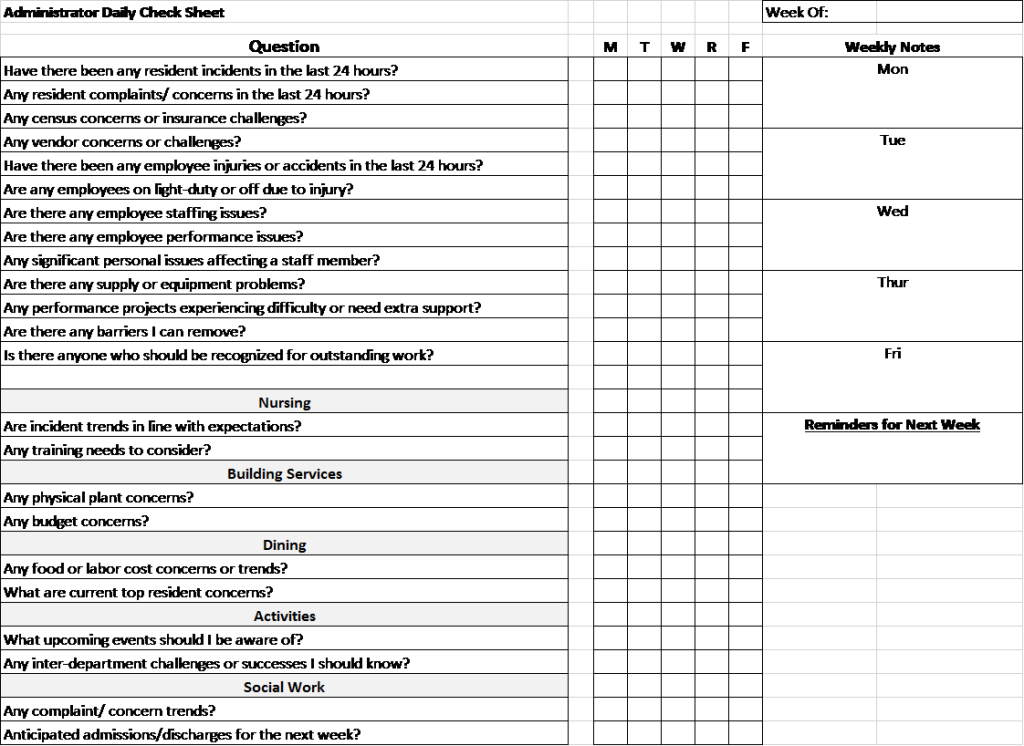
3) A Lack of Data Governance Structures
Very little literature has been written or developed regarding data governance in long-term care, and it’s likely that most providers do not have a formalized process for managing the integrity of data entered into an EHR, resulting in unnecessary variation, lowered resident outcomes, and less useful analytics and performance measures. To remedy this, providers need to develop a model for data governance and create processes to define and manage the information entered into the EHR. This means defining roles and responsibilities around the data that is entered, and developing systems and practices to standardize and sustain the data. Compliance should be measured on an ongoing basis, and frequent adjustments should be implemented as new needs are identified.
4) Failure to Embrace Optimization Opportunities
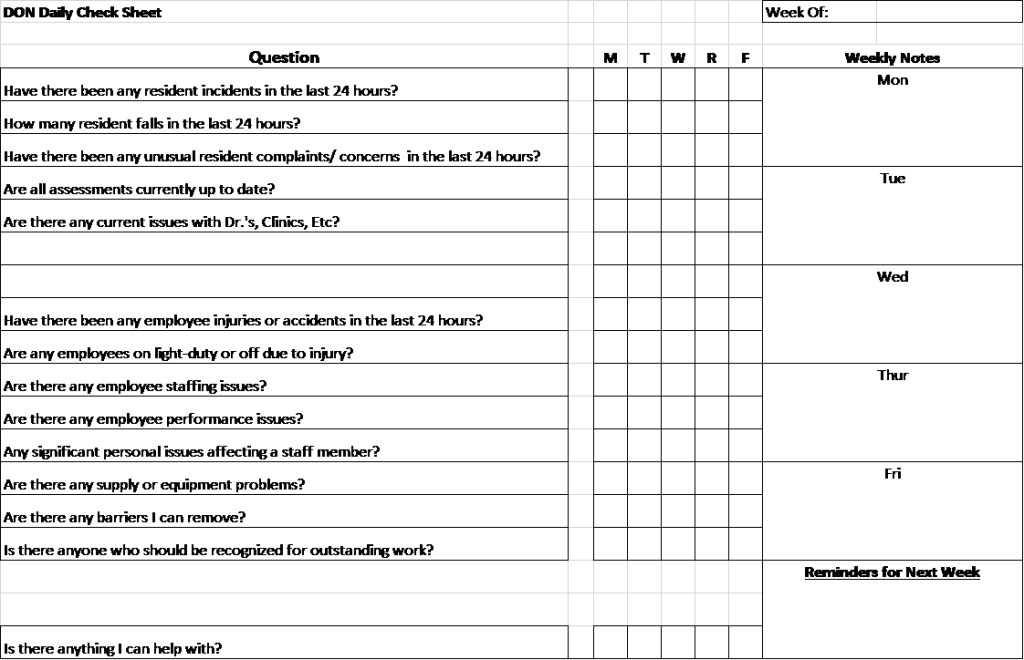
Optimization is the ongoing process of evaluating, improving, and sustaining an EHR over the product life-cycle. For many providers, however, an EHR simply becomes part of the background infrastructure after implementation is complete. For workflows that were not redesigned during implementation, extra or unneeded work often continues indefinitely. Workarounds to problematic features are typically developed and shared by floor staff, which can circumvent opportunities for useful analytics and reporting. In addition, new features developed by vendors are sometimes under- or un-utilized as they are typically buried in pages of product announcements and updates that are rarely viewed. In fact, it is not uncommon for legacy users– those who have had systems the longest– to be among the vendors’ lowest utilizers.
Providers should develop an ongoing optimization strategy that includes frequent observations of staff usage, regular discussions with the EHR vendor on new and planned enhancements, and collaboration with other users to discuss issues, workarounds, and innovative practices.
Have a little more time? Check out this excellent webinar from HIStalk on adoption success factors.
Considering an Electronic Health Record system for your nursing home or assisted living community? Looking to optimize a current installation? Learn how we can help with our EHR Consulting Services.