Are you struggling to accomplish your desired strategy? Thwarted by constant operational challenges? Your measurement systems might be able to help more– or they might even be part of the problem.
Many healthcare organizations track enormous amounts of data to guide their action and strategy. Sometimes, however, the pursuit of measures and metrics interfere with the implementation of strategy, and organizations struggle to move past the day-to-day business challenges to accomplish their long-term goals. Balanced scorecards and KPIs are two tool sets that, when used properly, can be used to facilitate both managing operations and preparing for future work.
Balanced Scorecards
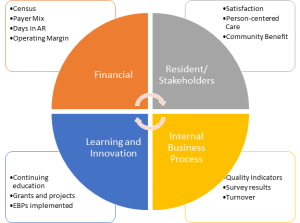
The concept of a balanced scorecard was developed in the mid-90s by Robert Kaplan and David Norton (with help from Art Schneiderman, et al.) as a response to the over-dependence on financial measures to guide organizational action. The purpose was to translate strategy into measures that could inform action by balancing financial measures with measures around the perspectives of customers, internal business processes and innovation/ learning. Over time, additional features were added, such as strategy maps to help visualize direction, and destination statements to provide more definition around goals.
A key challenge to implementing balanced scorecards is they take a significant investment of senior leadership’s time to develop. While financial measures are easy to translate across organizations (census, payer mix, days in AR and financial ratios would be common in long-term care), as well as some internal business measures (quality indicators, survey and cert. results), the customer and innovation quadrants needs to be more locally refined. Some organizations, for instance, serve specific populations, and the measures of success need to be closely aligned with those missions. Similarly, learning and innovation is important in every organization, but the actualization can vary from an interest in employee development to implementing evidence-based practices to technological adoption.
Sometimes, the challenge is having vague ideas about strategy but no clue about how to get there. I’ve worked for and with several organizations that have wanted to “be the best place to live and work” and “a teaching and learning organization.” They struggled year after year with making progress, however, because they didn’t hone in on specific measures to drive that strategy, nor did they have clear ideas about what exactly those lofty goals meant.
The Capital Care Group in Canada implemented a balanced scorecard, and there are some great lessons learned from research on that process:
“The balanced scorecard has focused on its role as a strategic management tool. The indicators and dimensions need to be customized to the organization. Senior management must be seen to be driving its introduction. It is worth spending sufficient time developing and implementing a scorecard rather than trying to rush its introduction. The scorecard needs to be integrated with existing management processes and sufficient resources must be assigned. However, success will ultimately depend on the culture of the organization being appropriate and receptive.”
Key Performance Indicators (KPIs)
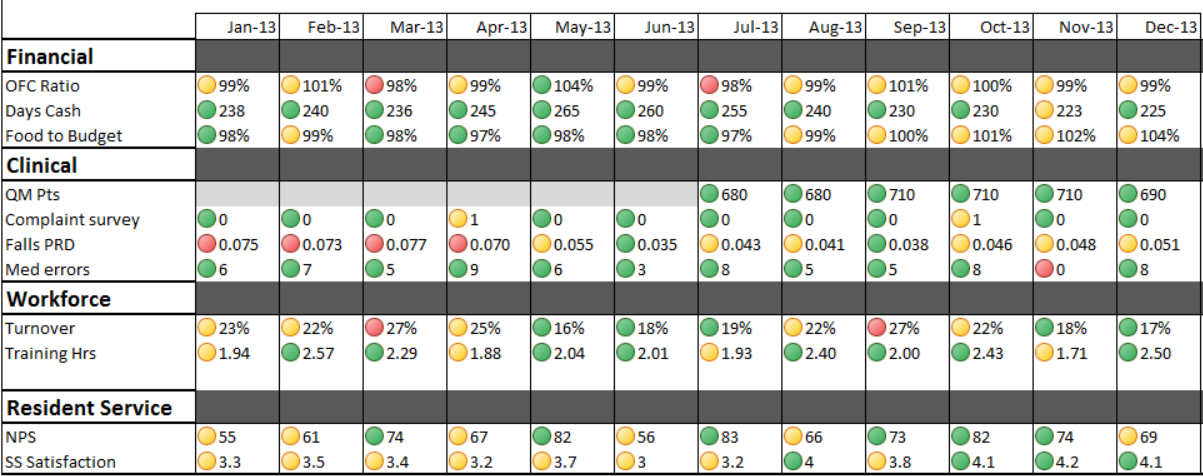
KPIs were developed to focus attention on accomplishing organizational strategy by measuring discrete data points. Again, financial measures have been used successfully for quite some time, but KPIs expand the reach to things like productivity, marketing success, turnover, meaningful quality measures (ones that either impact action or reflect operational results) and the like.
When adopting KPIs, it’s important to choose a limited number so that staff don’t become overwhelmed with the measurement of data for its own sake. It’s also important to understand the tendency for measured indicators to pervert performance by allowing managers to manipulate action in promotion of measured activities even at the expense of organizational success. I frequently see this when organizations measure turnover without regard to other performance metrics. This tends to incentivize managers to keep staff regardless of performance or actions– even at the detriment of team morale and operational effectiveness. High turnover is a costly problem in long-term care, for sure, but not all turnover is bad.
Using Organizational Metrics Effectively
Whatever system of measurement you use, it’s important to understand the systems themselves don’t determine strategy. Measurement systems are oftentimes compared to an automobile’s dashboard or an airplane’s cockpit: but remember, you can’t tell where you’re going, or, even moreso, what you’re supposed to do when you get there, by looking at a dashboard; nor can you tell whether you should go through an intersection by staring at your dash. Instead, the dashboard helps keep you on track and can highlight problems that might interfere with your trip. Balanced scorecards and KPIs function in a very similar way: they guide action and help implement strategy– but you still need to know where you are going and what you want to do when you get there, and you must keep in mind that they are only a piece of the overall operational puzzle.
eSSee Consulting has extensive experience developing and implementing measuring and metric systems in long-term care organizations. If you’re unhappy with your current system, or don’t have effective dashboards at all, we would love to help simplify your life by focusing on measures that truly impact performance and push you towards your desired goals.